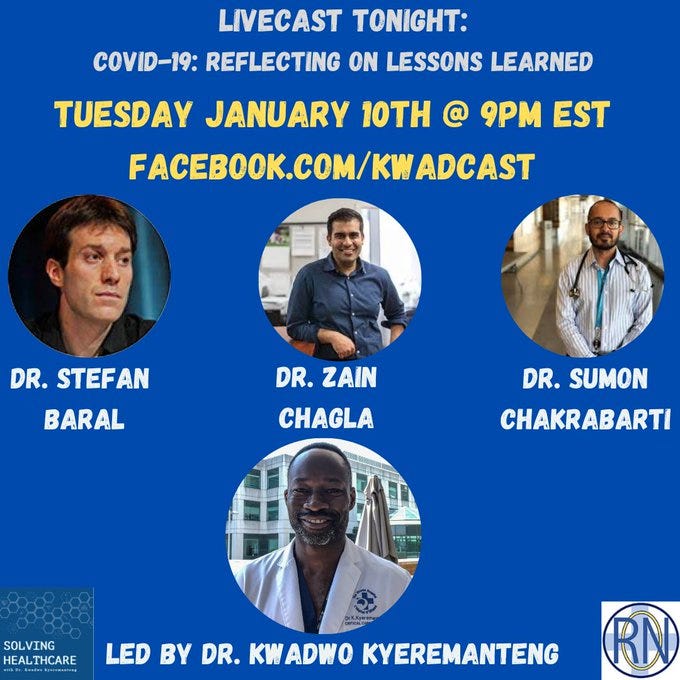
#220 Lessons From The Pandemic with Drs. Chagla, Baral & Chakrabarti (The Last Dance)
Episode Summary
In this livecast episode, we welcome back Dr. Zain Chagla, Dr. Stefan Baral, and Dr. Sumon Chakrabarti to address some of the issues we’ve seen throughout the pandemic, new variants and what to expect with future variants, discussing what we’ve done well over the past few years, misinformation, the effect of social media and the messaging on Twitter, the role media plays and the influence of experts on policy, public health agencies, booster shots to combat new variants and who actually needs them, where we are at with public trust, and much more!
SHOW SPONSOR
BETTERHELP
BetterHelp is the largest online counselling platform worldwide. They change the way people get help with facing life’s challenges by providing convenient, discreet and affordable access to a licensed therapist. BetterHelp makes professional counselling available anytime, anywhere, through a computer, tablet or smartphone.
Sign up today: http://betterhelp.com/solvinghealthcare and use Discount code “solvinghealthcare”
Thanks for reading Solving Healthcare with Dr. Kwadwo Kyeremanteng! Subscribe for free to receive new posts and support my work.
Thank you for reading Solving Healthcare with Dr. Kwadwo Kyeremanteng. This post is public so feel free to share it.
Transcript:
KK: Welcome to ‘Solving Healthcare’ I’m Kwadwo Kyeremanteng. I’m an ICU and palliative care physician
here in Ottawa and the founder of ‘Resource Optimization Network’ we are on a mission to transform
healthcare in Canada. I’m going to talk with physicians, nurses, administrators, patients and their
families because inefficiencies, overwork and overcrowding affects us all. I believe it’s time for a better
health care system that’s more cost effective, dignified, and just for everyone involved.
KK: All right, folks, listen. This is the first live cast that we have done in a very long time, probably a year.
Regarding COVID, we’re gonna call it a swan song, folks, because I think this is it. I’m gonna be bold and
say, this is it, my friends. I think what motivated us to get together today was, we want to learn, we
want to make sure we learned from what’s gone on in the last almost three years, we want to learn that,
in a sense that moving forward the next pandemic, we don’t repeat mistakes. We once again, kind of
elevate the voices of reason and balance, and so on. So, before we get started, I do want to give a
couple of instructions for those that are online. If you press NL into the chat box, you will be able to get
this. This recording video and audio sent to you via email. It’ll be part of our newsletter. It’s ballin, you’ll,
you’ll get the last one the last hurrah or the last dance, you know I’m saying second, secondly, I want to
give a quick plug to our new initiative. Our new newsletters now on Substack. Everything is on there
now our podcasts our newsletter. So, all the updates you’ll be able to get through there. I’m just going
to put a link in the chat box. Once I find it. Bam, bam, bam. Okay, there we go. There we go. That’s it
right there, folks. So, I feel like the crew here needs no introduction. We’re gonna do it. Anyway, we got
Dr. Zain Chagla, we got Dr. Stef Baral, we got Dr. Sumon Chakrabarti back in full effect. Once again, like I
said, we were we chat a lot. We were on a on a chat group together. We were saying how like, we just
need to close this out, we need to address some of the issues that we’ve seen during the pandemic. Talk
about how we need to learn and deal with some of the more topical issues du jour. So, I think what we’ll
start with, well get Sumon to enter the building. If you’re on Twitter, you’re gonna get a lot of mixed
messages on why you should be fearful of it or why not you should be fearful of it. So, from an ID
perspective, Sumon what’s your what’s your viewpoint on? B 115?
SC: Yeah, so, first of all, great to be with you guys. I agree, I love doing this as a as a swan song to kind of
move to the next stage that doesn’t involve us talking about COVID all the time. But so yeah, I think that
we’ve had a bit of an alphabet soup in the last year with all these variants. And you know, the most one
of the newest ones that we’re hearing about recently are BQ 1, xBB. I think that what I talked about
when I was messaging on the news was taking a step back and looking at what’s happened in the last 14
months. What that is showing us is that we’ve had Omicron For this entire time, which suggests a level
of genomic stability in the virus, if you remember, variants at the very beginning, you know, that was
synonymous with oh, man, we’re going to have an explosion of cases. Especially with alpha for the GTA
delta for the rest of, of Ontario, and I’m just talking about my local area. We saw massive increases in
hospitalizations, health care resources, of patients having been sent all over the province. So, it was it
was awful, right. But you know, I think that was a bit of PTSD because now after anybody heard the
word variant, that’s what you remember. As time has gone on, you can see that the number of
hospitalizations has reduced, the number of deaths has reduced. Now when omicron came yeah, there
was an explosion of cases. But you know, when you look at the actual rate of people getting extremely ill
from it, it’s much, much, much less. That was something that, you know, many of us were secretly
thinking, Man, this is great when this happened. So now where we are is we’re in January 2023, we’ve
had nothing but Omicron, since what was in late November 2020, or 21? Maybe a bit later than that.
And x BB, if you remember, be a 2x BB is an offshoot of BH two. Okay. Yeah, if you’re noticing all these
new variants are their immune evasive, they tend to be not as they’re not as visually as, I see this in my
own practice, like all of us do here. You know, they are, well, I’m kind of piecemeal evolution of the
virus. Now, there’s not one variant that’s gonna blow all the other ones out of the water, like Oh, micron
did or delta. Right. I think this is a good thing. This is showing that we’re reaching a different stage of the
pandemic, which we’ve been in for almost a year now. I think that every time we hear a new one, it
doesn’t mean that we’re back to square one. I think that this is what viruses naturally do. And I think
putting that into perspective, was very important.
KK: Absolutely. Zain just to pick your brain to like, I got this question the other day about, like, what to
expect what future variants like, obviously, is there’s no crystal ball, but someone alluded to the idea
that this is what we’re to expect. You feel the same?
ZC: Yeah, absolutely. It’s interesting, because we have not studied a Coronavirus this much, you know, in
history, right. Even though we’ve lived with coronaviruses, there probably was a plague of
coronaviruses. What was the Russian flu is probably the emergence of one of our coronaviruses are
seasonal coronaviruses. You know, I think we had some assumptions that Coronavirus is when mutate,
but then as we look to SARS, cov two and then we look back to see some of the other Coronavirus has,
they’ve also mutated quite a bit too, we just haven’t, you know, put names or other expressions to
them. This is part of RNA replication of the virus is going to incorporate some mutations and survival of
the fittest, the difference between 2020, 2021, 2022, and now 2023 is the only pathway for this virus to
keep circulating is to become more immune evasive. This is what we’re seeing is more immune evasion,
we’re seeing a variant with a couple more mutations where antibodies may bind a little bit less. But I
think that the big difference here is that that protection, that severe disease, right, like the COVID, that
we saw in 2020/2021, you know, that terrible ICU itis, from the COVID, you know, for the level of
antibody T cell function, non-neutralizing antibody functioning mate cell function, all of that that’s built
into, you know, humanity now through infection, vaccine are both really, you know, the virus can evolve
to evade some of the immunity to cause repeat infections and, you know, get into your mucosa and
replicate a bit, the ability for the virus to kind of, you know, cause deep tissue infection lead to ARDS
lead to all of these complications is getting harder and harder and harder. That’s us evolving with the
virus and that’s, you know, how many of these viruses as they emerge in the population really have kind
of led to stability more than anything else? So, yes, we’re going to see more variants. Yes, you know, this
is probably what what the future is, there will be some more cases and there may be a slight tick in
hospitalizations associated with them. But again, you know, the difference between 2020/2021/2022/
2023 is a syrup prevalence of nearly 100%. One way or another, and that really does define how this
disease goes moving forward.
KK: Yeah, absolutely. Maybe Stef we could pipe it a bit on, the idea that, first of all, I just want to
reinforce like as an ICU doc in Ottawa with a population of over a million we really have seen very little
COVID pneumonia since February 2022. Very minimal and it just goes to show know exactly what
Sumon and Zain were alluding to less virulent with the immunity that we’ve established in the
community, all reassuring science. One question I want to throw towards Stef, before getting into it. You
did an interview with Mike Hart. As you were doing this interview, I was going beast mode. I was hearing
Stef throw down. I don’t know if you were, a bit testy that day, or whatever. There was the raw motion
of reflecting on the pandemic, and how we responded and far we’ve gone away from public health
principles, was just like this motivator to say, we cannot have this happen again. I gotta tell you, boys,
like after hearing that episode, I was like ‘Yeah, let’s do this’. Let’s get on. Let’s go on another, do
another show. I’m gonna leave this fairly open Stef. What has been some of the keyways we’ve
approached this pandemic that has really triggered you?
SB: Yeah, I mean, so I guess what I’d say is, in some ways, I wish there was nobody listening to this right
now. I wish there was like, I don’t know what the audience is. I don’t know if it’s 10 people or under
people, but I think it’s like, I wish nobody cared anymore. I want Public Health to care. I want doctors to
care, we’re going to keep talking because you know, Kwadwo, you’ve had folks in the ICU we we’ve
we’ve seen cases in the shelters, we have outbreaks, like public health is always going to care about
COVID, as it cares about influenza cares about RSV, and other viruses, because it needs to respond to
outbreaks among vulnerable folks. That will never stop COVID, it was just clear very early, that COVID is
going to be with us forever. So that means tragically, people will die of COVID people. I think that, you
know, there’s that that’s a reality, it’s sometimes it’s very close to home for those of us who are
providers, as it has for me in the last week. So COVID never ends. I think the issue is that like when does
COVID And as a matter of worthy of discussion for like the average person? The answer is a long time
ago. I mean, I think for the folks that I’ve spoken to, and the way that we’ve lived our lives as a family is
to focus on the things that like bring folks joy, and to kind of continue moving along, while also ensuring
that the right services are in place for folks who are experiencing who are at risk for COVID and serious
consequences of COVID. Also just thinking about sort of broader systems issues that I think continue to
put folks at risk. So, one: I think it’s amazing, like how little of the systematic issues we’ve changed,
we’ve not improved healthcare capacity at all. Amazingly, we’ve not really changed any of the structures
that put our leg limitations on the on the pressures on the health system, none of that has changed. All
of it has been sort of offset and downloaded and just like talking about masks and endless boosters
when we’ve never really gotten to any of the meaty stuff. As you said three years into it, and
everybody’s like, well, it’s an emergency. I’m like, it was an emergency and fine. We did whatever was
needed, even if I didn’t agree with it at the time. But irrespective of that, whatever that was done was
done. But now it’s amazing that like the federal money expires for COVID In next few months, and all
well have shown for this switch health guys got became millionaires like a bunch of people, I don’t mind
naming and I don’t care anymore. These folks, these Grifters went out and grabbed endless amounts of
money. These cash grabs that arrival, the ArriveCan app with, like these mystery contractors that they
can’t track down millions of dollars. So it’s like all these folks like grabbed, you know, huge amounts of
money. And I think there’s a real question at the end of it of like, what are we as a country? Or you
know, across countries? What do you have to show for it? How are you going to better respond? And
the answer right now is like very little, like we have very little to show for all this all these resources that
have been invested, all this work that has been done. That I think should be the conversation. That to
me needs to be this next phase of it is like billions and billions and billions of dollars trillion or whatever,
like 10s of billions of dollars were spent on what? and what was achieved? And what do we want to do
next time? And what do we have to show for it? that, to me feels like the meat of the conversation
rather than like silly names for these new variants that do nothing but scare people in a way that isn’t
helpful. It does not advance health. It doesn’t you know, make the response any more helpful. It just
scares people in a way that I think only detracts them from seeking the care that we want them to be
seeking.
KK: Yeah, I think you brought up a point to about or alluded to how some of this was the distraction.
That was one of the points that really stuck home is that we, we didn’t really dive into the core s**t, the
core issues. This is why at the end of it all, are we that much more ready for the next pandemic that well
see, you know, and so like maybe Sumon, what do you think in terms of another tough one, are we
ready for the next pandemic? Do you think we’ve done enough? do we think are in terms of what we’ve
invested in, how we’ve communicated to the public. The messaging to the public. Are we learning? Is my
question, I guess.
SC: I’m a clinician and I don’t work with the public health and the policy aspect as closely as Stefan does.
But I will say that, obviously, I’ve been in this realm for quite a long time, since in ID, I think that, you
know, what that’s important to remember is that for SARS 1 we actually had this document that
outlined all of this, you know, masking, social distancing, what to do with funding and all that kind of
stuff. Basically, I was actually interviewed about this, I remember back way back in 2020, and half of it
was basically just thrown out the window. I think that a lot of what happened is that fear came in
decisions were made from emotion, which is, by the way, understandable, especially in April 2020. I’ve
shared with you guys before that, in February 2020, I was waking up at night, like nervous, that I was
gonna die. I that that’s where I was thinking I it was, it was terrible. I completely understand making
those decisions. I think as time went on, I wish that, you know, there’s a bit more of public health
principles. You know, making sure that we’re dealing with things without, you know, stepping on
people’s bodily autonomy, for example, you know, doing things in an equitable way, where you, you
know, we all know that every intervention that you do is squeezing a balloon, you must remember the
unintended consequences, I think that we did. So, kind of putting that all together. I think, right now, as
we stand in Canada if we do have another pandemic. I fear that a lot of these same mistakes are going
to be made again, I should say, a disruptive pandemic of this because it’s not forgotten H1N1, the
pandemic it that was a pandemic, right. It wasn’t nearly as disruptive as COVID was, but I do think that
inquiry and like you mentioned at the beginning, Kwadwo was talking about what we did, well, we didn’t
do well, and making sure the good stuff happens, and the bad stuff doesn’t happen again, because this is
likely not the last pandemic, in the information age in our lifetimes.
KK: Zain, was there anything that stuck out for you? In terms of what you’d really want to see us
improve? Or whether it is messaging, whether it is public health principles, does any of those stick out in
your mind?
ZC: Yeah, I mean, I think the one unique thing about this pandemic that is a lesson moving forward and
for us to kind of deal with I think we talked about messaging. This was the first major pandemic that
occurred with social media and the social media era, right, and where, information, misinformation,
disinformation, all the things that were all over the place, you know, we’re flying, right, and there does
need to be some reconciliation of what’s been we have to have some reconciliation of some of the
benefits of the social media era in pandemic management, but also the significant harms the people,
you know, we’re scared that people got messaging that may not have been completely accurate, that
people had their biases as they were out there. I will say even that social media component penetrated
into the media. This is also the first time that I think we saw experts you know, including myself and
Suman and all of us you know, that you know, could be at home and do a news interview on National
News in five minutes and be able to deliver their opinion to a large audience very quickly. So, you know,
I think all of that does need a bit of a reconciliation in terms of what worked, what doesn’t how you
validate you know, good medical knowledge versus knowledge that comes from biases how we evaluate
psi comm and people you know, using it as a platform for good but may in fact be using it you know,
when or incorporating their own biases to use it for more, more disinformation and misinformation
even if they feel like they have good intentions with it. I you know, I think this is a, you know, for the
sociologists and the communications professionals out there, you know, really interesting case example
and unfortunately, I don’t think we came out the other side. Social media being a positive tool, it may
have been a positive tool, I think in the beginnings, but, you know, I think I’m finding, it’s nice to
communicate with folks, but I’m finding more harm and more dichotomy and division from social media
these days is compared to the beginnings of the pandemics where, you know, I think, again, there’s just
been so much bias, so much misinformation so much people’s clouds and careers that have been, you
know, staked on social media that it’s really become much, much harder to figure out what’s real and
what’s not real in that sense.
KK: Absolutely, I fully agree Zain. At the beginning, in some ways, I’ll tell you, ICU management, that
whole movement for us to delay intubation, as opposed to intubation early, I really think it was pushed
by in social media. So, I think it saved lives, right. But then, as we got through more and more the
pandemic, wow, like it, like the amount of just straight up medieval gangster s**t that was going on that
in that circle, in that avenue was crazy. Then just like, I mean, this might be controversial to say, I don’t
know, but news agencies got lazy, they would use Twitter quotes in their articles as, evidence, or as
proof of an argument. It’s like, what is happening? It? Honestly, when you think about it, it was it was
crazy. It still is crazy.
ZC: Yeah. And I think expertise was another issue. Right. And, you know, unfortunately, we know of, you
know, certain experts that were not experts that weren’t certified that weren’t frontlines and a variety
of opinions and various standpoints and epidemiology, public health, intensive care, infectious diseases,
whatever is important. But, you know, there were individuals out there that had zero experience that
were reading papers and interpreting them from a lens of someone that really didn’t have medical
experience or epidemiologic experience, that chased their clout that made money and, we know some
examples that people that eventually had the downfall from it, but you know, at the end of the day,
those people were on social media, and it penetrated into real media, and then that is a real lesson for
us is that validation of expertise is going to be important. You know, as much as we allow for anyone to
have an opinion, you know, as they get into kind of real media, they really have to be validated that that
opinion comes from a place that’s evidence based and scientific and based on a significant amount of
training rather than just regurgitating or applying one small skill set and being an expert in many other
things.
KK: Sumon
SC: So we’re just gonna add really quickly is that, in addition to what Zain saying. When this stuff bled
over from social media to media, the thing that I mean, at least what it seemed like is he was actually
influencing policy. That’s, I think that’s the important thing is, so you can have 10 people 20 people
yelling, it doesn’t matter if they’re extreme minority, if it’s influencing policy that affects all of us, right.
So, I think that’s important.
KK: I’ll be honest with you, like, I got to the point where I really hated Twitter, I still kind of hate Twitter.
Okay. It was conversation. I remember Sumon that you and I had I don’t remember it was we were
texting. I think we talked about this. But the fact that policy could be impacted by what we’re throwing
down the facts or the messages that we were doing on media that this can impact policy, you had to
like, especially when there was some badness happening, we had to step up. We had to be a voice of
logic, whether it was mandates, whether it was you know, lockdown school closures, whatever it might
have been like, the politicians, we heard about this politicians looking at this, the mainstream media
looking at this, and for us not to say anything at this point, like we had, we had to do something Sorry,
Stef, you’re gonna jump in?
SB: Yeah, I think I think what was interesting to me to see and I think a clear difference between H1N1
was that in a lot of places, and including in Ontario, across the US, where this sort of emergence of these
like the science tables, these task forces, these whatever you want to call them, it was like a new body
of people often whom had never spent a day in a public health agency. Often academics that you know,
are probably good with numbers, but really don’t have a lot of experience delivering services, you know,
all of a sudden making decisions. So I think there’s a real interesting dynamic that when you compare,
for example, Ontario and British Columbia, one has this science table one does not, and just how
different things played out, I mean, given it’s a, you know, an end of have to, or no one in each camp,
but I think what you see is like, there’s a place there where like public health or you know, let’s say,
Sweden, you know, as a public health agency that didn’t strike up its own taskforce that used its
traditional public health agency. I think was in a place to make more like reasoned and measured
decisions, and just was better connected, like the relationships exist between the local health
authorities and the provincial health authorities and the national ones. I think when you set up these,
the one thing that I hope we never do, again, is that something like the science table never happens
again. That’s not to sort of disparage most of the people. Actually, most of the folks on the science table
I like, and I respect, say many of them, maybe not most, but many of them, I like and respect, but it is
the case that there was it was they weren’t the right group of people. They weren’t representative
Ontarians he was like, ten guys and two women, I think, I don’t know many of them white, they weren’t
representative socio economically, racially diverse, anything. They didn’t have the right expertise on
there. I would have liked to see some like frontline nurses on there to say ‘listen, this stuff is silly’ or
some frontline, whoever just some frontline folks to be say ‘listen, none of the stuff that you’re saying
makes any sense whatsoever’. And luckily, there was some reason, voices on there, but they were the
minority. But luckily, they prevailed, or we would have had outdoor masking and even tougher
lockdowns. I don’t know how folks really; it was really close. I think we fortunately had that
representation, but that should have never even happened, we should have had public health Ontario,
being its agency and making recommendations to the ministry and to the government. There should
have never been a science table. Then second thing, I just want to say I’ve we’ve talked about this
forever and I do think we should talk about this more, not in the context of like this, this podcast, but is
also just absolutely the role of the media. I do want to say that, like historically, media had to do a lot of
work, they had to go to universities or hospitals and ask for the right expert, and then the media or
comms team, ‘you should really talk to Zain Chagla’ Because he has good example, you know, it gives
good expertise on this or you start to like, I don’t know, like Dr. so and so for this or that, and they put
together the right person, they organize the time and then they talk. Now you know that it was really
like the story I think was more organically developed on based on what the experts had to say. Now
you’ve got reporters, for people who are not from Ontario, there’s a sports reporter in the city of
Toronto that I looked historically, I can’t see that they’ve ever done anything in public health suddenly
became like the COVID reporter in the city of Toronto, for a major newspaper. It’s like this person has
not a clue of what they’re talking about, just like has no clue they’ve never trained in. I don’t disparage
their sports reporter like why should they? but they became the voice of like public health for like the
average person. It just it set us up where that person just had a story and then just found whatever
people on Twitter that they could to like back up their story irrespective to drive controversy, to drive
anger towards the government based on sort of political leanings. Even if maybe my political leanings
are aligned with that person, it’s a relevant because it’s not about politics, it’s about public health. So I
think the media, we have to think about, like, how do we manage the media’s need for clicks and profit,
you know, during this time, in with, like, their role as like, the responsible are an important part of like,
you know, social functioning, in terms of the free press. So, I, there’s no easy answers to that. But I’ll just
say, I think there was a fundamentally important role that the media played here. And I have to say, it
didn’t play out positively, in most places.
KK: I gotta say, like, this is gonna be naive talk. But we’re in a pandemic, there had to be so many of us
had a sense of duty, like, I was surprised at the lack of sense of duty, to be honest with you. Even if you
are about your cliques, ask yourself, is this is this about the greater good here? Is this really gonna get us
further ahead? I’ve said this a few times on my platform, I would have a balance of a mess. The balanced
message on was usually one specific network that would bail on the interview. They would literally bail
on the interview because my message might not be as fearful. What the actual f you know what I mean?
Like it’s crazy.
(?) I will say there were some good reporters. I don’t want to say that that you know, there were some
incredible folks. I was talking to someone the other day, I won’t mention who but I think the mark of the
good reporter was, you know, they have a story, they want to talk about it. They contacted us. And they
said, what time can we talk this week, right? They didn’t say I need to get this filed in three hours. If you
say you need to get this filed in three hours, the expert you’re gonna go to is the one that’s available in
the next three hours, right? They wanted to hear an opinion, they wanted to get multiple opinions on
the table, but they would carve out the time so that everyone could give their story or, what their
opinion was or what evidence they presented. They made sure it rotated around the experts rather than
the story rotating around being filed. I think it’s important and, you know, you can get a sense of certain
things that are on the need to be filed this day, or even on the 24/7 news cycle, where they may not be
as well researched, they’re they’re a single opinion. They’re quoting a Twitter tweet. Now, I think in
some of these media platforms, you can just embed that Twitter tweet, you don’t even have to, you
know, quote it in that sense, you just basically take a screenshot of it basically. Versus again, those
articles where I think there was there more thought, and I think there were some great reporters in
Canada, that really did go above and beyond. Health reporters, particularly that really did try to present
a picture that was well researched, and evidence based, you know, with what’s available, but there
certainly are these issues and it’s not a COVID specific issue, but with media ad reporting, in that sense.
Yeah, it’s and it’s important to say like, it’s not actually just the reporter, it’s the editors, its editorial
teams, like I had said, OTR discussions with reporters very early on, I’ve tried to stay away from the
media, because I think the folks who have done it, I’ve done it well. But it was interesting, because Bob
Sargent, who sadly passed away, an internal medicine physician, and an amazing mentor to many
clinicians in Toronto. Put me in touch with a couple of reporters. He’s like, you know, you’re a public
health person, you should really talk to these reports. We had this; can we talk to you privately? It was
so weird. This was summer of 2020. So, we had a very private discussion where I said ‘Listen, I have
concerns about lockdowns for like, these reasons’ I think it’s reasoned, because it’s not it, I’ve got no
conspiracy to drive, like, I’ve got no, there’s no angle in any of it. So, but it was just fascinating. So, they
were like we might be able to come back to you, and maybe we’ll try to do a story around it. Then they
came back and said, we’re not going to be able to pursue it. I said that’s fine. It’s no problem. It just sort
of showed that I think, similar as academics, and clinicians, and all of us have been under pressure based
on everything from like CPSO complaints, the complaints to our employers, to whatever to just saw, you
know, the standard attacks on Twitter. I think there was also a lot of pressure on reporters based on this
whole structure, and of it. So I think, I don’t mean to disparage anybody, but I do think the point that
you made is really important one is. I’ll just say, in our own house, you know, my wife and I both were
like talking at the beginning of this and being like, what do we want to know that we did during this
time? So, my wife worked in person, as a clinician alter her practice all throughout her pregnancy? She
never didn’t go, you know, she did call she did all of that, obviously, I have done the work I’ve done in
terms of both clinically and vaccine related testing. But this just idea of like, what do you want to
remember about the time that you would like what you did when s**t hit the fan? And, you know,
because first, it’ll happen again, but just also, I think it’s important to sort of, to be able to reflect and
think positively about what you did. Anyways,
KK: I hear you both, part of it, too, for me, I’ll just straight up honesty. In some ways, I’m just pissed, I’m
pissed that a lot of the efforts that were that a lot of people put into to try and get a good message out
there. The backlash. Now people reflecting saying, ‘Oh, I guess you did, you know, many of you do to
had a good point about lockdowns not working out’. I know it may be childish in some way, but it’s just,
you know, a lot of us have gone through a lot to just try and create a balanced approach. I think there
was a little bit of edge in this voice, but I think it comes with a bit of a bit of reason to have a bit of edge.
I think in terms of the next couple questions here are areas to focus on. A lot of people in terms of like,
decisions regarding mandates, boosters, and so forth, like we talk a lot about it on public health, it’s the
data that helps drive decisions, right. That’s really what you would think it should be all about. So, one of
the many questions that were thrown to us, when we announced that this was happening was, the need
for like, almost like universal boosters, and Sumon, I’ll put you on the spot there, at this stage in the
pandemic, where I’m gonna timestamp this for people on audio, we’re on January 10th, 2023. There are
some questions that we get, who really needs to push through to we all need boosters? What’s your
thoughts on that?
SC: So, I think that one of the things that I said this, as Zain makes fun of me throughout the pandemic, I
came up with catchphrases, and my one for immunity is the way that we’ve conceptualized immunity in
North America. I think a lot of this has to do with an actual graphic from the CDC, which likens immunity
to an iPhone or a battery, iPhone battery. So, iPhone immunity, where you have to constantly be
recharging and updating. I think that has kind of bled into the messaging. That’s what we think of it. I
remember back in I think it was October of 2021, where they were also starting to talk about the third
dose. The third dose, I think that at that time, we knew that for the higher risk people, it was probably
the people who would benefit the most from it. We had Ontario data from it was I think, was ISIS.
There’s vaccine efficacy against hospitalization, over 96% in Ontario in health care workers 99%, if you’re
less than seventy-seven years of age, yet this went out, and everybody felt like they had to get the
booster. So, I think that the first thing that bothered me about that is that there wasn’t a kind of
stratified look at the risk level and who needs it? So now we’re in 2023. I think that one of the big things
apart from what I said, you know, who’s at higher risk, there’s still this problem where people think that
every six months, I need to recharge my immunity, which certainly isn’t true. There wasn’t a recognition
that being exposed to COVID itself is providing you a very robust immunity against severe disease, which
is kind of it’s coming out now. We’ve been we’ve all been talking about it for a long time. And you know,
the other thing is that the disease itself has changed. I think that I heard this awesome expression, the
first pass effect. So, when the COVID first came through a completely immune naive population, of
course, we saw death and morbidity, we saw all the other bad stuff, the rare stuff that COVID
encephalitis COVID GB GBS tons of ECMO, like 40-year old’s dying. With each subsequent wave as
immunity started to accrue in the population, that didn’t happen. Now we’re at a different variant. And
the thing is, do we even need to be doing widespread vaccination when you’re with current variant, and
you can’t be thinking about what we saw in 2021. So, putting that now, all together, we have as Zane
mentioned, seroprevalence, about almost 100%, you have people that are well protected against severe
disease, most of the population, you have a variant that absolutely can make people sick. And yes, it can
kill people. But for those of us who work on the front line, that looks very different on the on the front
lines. So, I really think that we should take a step back and say, number one: I don’t think that the
booster is needed for everybody. I think number two: there are under a certain age, probably 55 and
healthy, who probably don’t need any further vaccination, or at least until we have more data. Number
three: before we make a widespread recommendation for the population. We have time now we’re not
in the emergency phase anymore. I really hope that we get more RCT data over the long term to see
who is it that needs the vaccine, if at all. And you know, who benefits from it. And let’s continue to
accrue this data with time.
KK: Thanks Sumon. Zain, are you on the along the same lines assume on in terms of who needs boosters
and who doesn’t?
ZC: Yeah, I mean, I think number one: is the recognition that prior infection and hybrid immunity
probably are incredibly adequate. Again, people like Paul Offit, and we’re not just talking about you
know, experts like us. These are people that are sitting on the FDA Advisory Committee, a man that
actually made vaccines in the United States, you know, that talks about the limitations of boosters and
probably three doses being you know, The peak of the series for most people, and even then, you know,
two plus infection probably is enough is three or even one plus infection, the data may suggest maybe is
as high as three. Yeah, I think, again, this is one of these things that gets diluted as it starts going down
the chain, if you actually look at the Nazi guidance for, you know, bi-Vaillant vaccines, it’s actually
incorporates a ‘should’ and a ‘can consider’ in all of this, so they talked about vulnerable individuals,
elderly individuals should get a booster where there may be some benefits in that population, the rest
of the population can consider a booster in that sense, right. And I think as the boosters came out, and
again, you know, people started jumping on them, it came to everyone needs their booster. And
unfortunately, the messaging in the United States is perpetuated that quite a bit with this iPhone
charging thing, Biden tweeting that everyone over the age of six months needs a booster. Again, we
really do have to reflect on the population that we’re going at. Ultimately, again, if you start pressing the
issue too much in the wrong populations, you know, the uptake is, is showing itself, right, the people
who wanted their bi-Vaillant vaccine got it. Thankfully the right populations are being incentivized,
especially in the elderly, and the very elderly, and the high risk. Uptake in most other populations has
been relatively low. So, people are making their decisions based on based on what they know. Again,
they feel that that hesitation and what is this going to benefit me? and I think as Sumon said, the
confidence is going to be restored when we have better data. We’re in a phase now where we can do
cluster randomized RCTs in low-risk populations and show it If you want the vaccine, you enter into a
cluster randomized RCT, if you’re in a low-risk population, match you one to one with placebo. You we
can tell you if you got, you know, what your prognosis was at the end of the day, and that information is
going to be important for us. I don’t think that policy of boosting twice a year, or once a year is gonna
get people on the bus, every booster seems like people are getting off the bus more and more. So, we
really do have to have compelling information. Now, as we’re bringing these out to start saying, you
know, is this a necessity? especially in low-risk populations? How much of a necessity is that? How much
do you quantify it in that sense? And again, recognizing that, that people are being infected? Now, that
adds another twist in that sense.
KK: Yeah, and we’ll talk a little bit about public trust in a bit here. But Stef, you were among some
authors that did an essay on the booster mandates for university students. As we’ve both alluded to
Zain, and Sumon there’s this need to be stratified. From an RCT booster point of view that we’re not well
established here. When Stef’s group looked at university mandates and potential harm, when we’re
doing an actual cost benefit ratio there, their conclusion was that there’s more room for harm than
benefits. So, Stef I want you to speak to that paper a bit.
SB: Sure. So, I will say this, I don’t actually have much to add other than what Zain and Sumon said. Run
a vaccine program we are offering, you know, doses as it makes sense for folks who are particularly
immunocompromised, multiple comorbidities and remain at risk for serious consequences related to
COVID-19. We’ll continue doing that. And that will, you know, get integrated, by the way into like, sort
of a vaccine preventable disease program, so offering, shingles, Pneumovax, influenza COVID. And also
we want to do a broader in terms of other hepatitis vaccines, etc. That aside, so this, this isn’t about, you
know, that it was really interesting being called antivax by folks who have never gotten close to a
vaccine, other than being pricked by one. Having delivered literally 1000s of doses of vaccine, so it’s
almost it’s a joke, right? but it’s an effective thing of like shutting down conversation. That aside, I think
there’s a few things at play one as it related to that paper. I find it really interesting, particularly for
young people, when people are like, listen, yes, they had a little bit of like, inflammation of their heart,
but it’s self-resolving and self-limiting, and they’re gonna be fine. You don’t know that. Maybe sure we’ll
see what happens with these folks twenty years later. The reality is for younger men, particularly, this
happens to be a very gender dynamic. For younger men, particularly, there seems to be a dynamic
where they are at risk of myocarditis. I don’t know whether that’s a controversy in any other era for any
other disease, this would not be a controversy would just be more of a factual statement, the data were
clearer in I’d say, probably April, May 2021. I think there’s lots of things we could have done, we could
have done one dose series for people who had been previously infected, we could have stopped at two.
There are a million different versions of what we could have done, none of which we actually did. In the
context of mandating boosters now for young people, including at my institution, you were mandated to
get a booster, or you would no longer be working. So obviously, I got one. There’s a real dynamic of
what is it your goal at that point? because probably about 1011 months into the vaccine program
became increasingly clear. You can still get COVID. Nobody’s surprised by that. That was clear even from
the data. By the way, wasn’t even studied. I mean, Pfizer, the way if you just look at the Pfizer, Moderna,
trials, none and look to see whether you got COVID or not, they were just looking at symptomatic
disease. That aside, I think that it just became this clear thing where for younger men, one or two doses
was plenty and it seems to be that as you accumulate doses for those folks, particularly, it’s also
important, if somebody had a bad myocarditis, they’re not even getting a third dose. So, you’re already
selecting out, you know, some of these folks, but you are starting to see increased levels of harm, as it
related to hospitalization. That what we basically did, there was a very simple analysis of looking at
averted hospitalization, either way, many people say that’s the wrong metric. You can pick whatever
metric you want. That’s the metric we picked when terms of hospitalization related to side effects of the
vaccine versus benefits. What it just showed was that for people under the age of 30, you just don’t see
a benefit at that point, as compared to harm that’s totally in fundamentally different. We weren’t talking
about the primary series, and we weren’t talking about older folks. So indeed, I think, you know, that
was that was I don’t know why it was it was particularly controversial. We it was a follow up piece to
mandates in general. I’ll just say like, I’ve been running this vaccine program, I don’t think mandates
have made my life easier at all. I know, there’s like this common narrative of like mandates, you know,
mandates work mandates work. I think at some point, and I’ll just say our own study of this is like we’re
really going to have to ask two questions. One: what it mandates really get us in terms of a burden
COVID-19, morbidity, mortality? and two: this is an important one for me. What if we caught ourselves
in terms of how much pressure we put on people, as it relates to vaccines right now, in general? The
very common narrative that I’m getting is they’re like, oh, the anti Vax is the anti Vax folks are winning.
And people don’t want their standard vaccines, and we’re getting less uptake of like, MMR and
standard, you know, kind of childhood vaccines, I have a different opinion. I really do at least I believe
some proportion of this, I don’t know what proportion, it’s some proportion, it’s just like people being
pushed so hard, about COVID-19 vaccines that they literally don’t want to be approached about any
vaccine in general. So, I just think that with in public health, there’s always a cost. Part of the decision
making in public health as it relates to clinical medicine too. It’s like you give a medication, the
advantage and then you know, the disadvantages, side effects of that medication. In public health, there
are side effects of our decisions that are sometimes anticipated and sometimes avoidable, sometimes
can’t be anticipated and sometimes can’t be avoided. You have to kind of really give thought to each of
them before you enact this policy or you might cost more health outcomes, then then you’re actually
gaining by implementing it.
KK: Yeah, number one: What was spooky to me is like even mentioning, I was afraid even to use a term
myocarditis at times. The worst part is, as you said, stuff, it’s young folk that were alluding to, and for us
to not be able to say, let’s look at the harm and benefit in a group that’s low risk was baffling. It really
was baffling that and I’m glad we’re at least more open to that now. Certainly, that’s why I thought that
the paper that you guys put together was so important because it’s in the medical literature that we’re
showing, objectively what the cost benefit of some of these approaches are. Sumon: when you think of
mandates and public trust, that Stef was kind of alluding to like, every decision that we made
throughout this thing. Also has a downside, also has a cost, as Stef was mentioning. Where do you think
we are? In terms of the public trust? Talking about how the childhood vaccines are lower. I don’t know
what influenza vaccine rates are like now, I wouldn’t be surprised if they’re the same standard, but who
knows them where they’re at, currently. Based on your perspective, what do you think the public trust is
right now?
SC: Yeah, as physicians, we obviously still do have a lot of trust in the people we take care of. People are
still coming to see us. I wish they didn’t have to because everyone was healthy but that’s not the case. I
do think that over the last two and a half, we’re coming up on three years, I guess right now, that people
that we have burned a lot of trust, I think that mandates were part of it. I do think that some of it was
unavoidable. It’s just that there’s a lot of uncertainty. There was back and forth. I think that one thing
that were that concern me on social media was that a lot of professionals are airing their dirty laundry to
the public. You could see these in fights, that doesn’t, that’s not really a good thing. We saw people
being very derisive towards people who were not listening to the public health rules. You know what I
mean? There’s a lot of that kind of talk of othering. Yeah, I think that that certainly overtime, eroded
public trust, that will take a long time to get back, if we do get it back. I think that the bottom line is that,
I get that there are times that we have to do certain things, when you have a unknown pathogen coming
at you, when you don’t really know much about it. I do think that you want to do the greatest good for
the, for the population or again, you always must remember as Stefan alludes to the cost of what you’re
doing. I do think that we could have done that much early on. For example, Ontario, we were locked
down in some areas, Ontario, GTA, we were locked down in some regard for almost a year and a half. If
you guys remember, there was that debate on opening bars and restaurants before schools. It’s just like,
I remember shaking my head is, look, I get it, I know you guys are talking about people are going to be
eating a burger before kids can go to school, that might ruin everything. But the problem is, is that you
must remember that restaurant is owned by someone that small gym is someone’s livelihood, you’re
moralizing over what this is, but in the end, it’s the way somebody puts food on the table. For a year
and a half, we didn’t let especially small businesses do that. I’m no economist, but I had many family
members and friends who are impacted by this. Two of my friends unfortunately, committed suicide
over this. So, you know, we had a lot of impact outside of the of the things that we did that hurt people,
and certainly the trust will have to be regained over the long term.
KK: It’s gonna take work. I think, for me, honestly, it’s, it’s just about being transparent. I honestly, I put
myself in some in the shoes of the public and I just want to hear the truth. If we’re not sure about
something, that’s okay. We’re gonna weigh the evidence and this is our suggestion. This is why we’re
saying this, could we be wrong? Yes, we could be wrong but this is what we think is the best path
forward, and people could get behind that. I honestly feel like people could get behind that showing a
little bit of vulnerability and saying ‘you know, we’re not know it alls here’ but this is what our best
strategy is based on our viewpoint on the best strategy based on the data that we have in front of us
and just be open. Allowing for open dialogue and not squash it not have that dichotomous thinking of
you’re on one side, you’re on the other. You’re anti vax, you’re pro vax, stop with the labels. You know,
it’s just it got crazy, and just was not a safe environment for dialogue. And how are you supposed to he’s
supposed to advance.
SB: Yeah, I do want to say something given this this is this idea of our swan song. I think there was this
sort of feeling like, you know, people were like ‘you gotta act hard, you gotta move fast’ So I think
everybody on this, you guys all know I travel a lot. I like to think of myself as a traveler. In the early
2020’s I did like a COVID tour, I was in Japan in February, then I was in Thailand, and everywhere I
landed, there were like, COVID here, COVID here, COVID here. Then finally, I like got home at the end of
February, and I was supposed to be home for like four days, and then take off. Obviously things got shut
down. It was like obvious like COVID was the whole world had COVID by, February, there may have been
a time to shut down this pandemic in September 2019. Do you know what I mean? by November 2019,
we had cases. They’ve already seen some and Canadian Blood Services done some showing some
serological evidence already at that time. There was no shutting it down. This thing’s gonna suck. The
reality is promising that you can eliminate this thing by like, enacting these really like arbitrary that can
only be described as arbitrary. Shutting the border to voluntary travel, but not to truckers. Everything
felt so arbitrary. So, when you talk about trust, if you can’t explain it, if you’re a good person do it. If you
don’t do it, your white supremacist. Kwadwo you were part of a group that was called ‘Urgency of
Normal’ you are a white supremacist. It’s so ridiculous. You know what I mean? It creates this dynamic
where you can’t have any meaningful conversation. So, I really worry, unless we can start having some
really meaningful conversations, not just with folks that we agree with. Obviously, I deeply respect what
each of you have done throughout this pandemic, not just actually about what you say, but really what
you’ve done. Put yourselves out there with your families in front of this thing. That aside, if we can’t do
that, we will be no better off. We will go right back. People will be like ‘Oh, next pandemic, well, let’s
just get ready to lock down’ but did we accomplish anything in our lock downs? I actually don’t think we
did. I really don’t think we got anything positive out our lock downs, and I might be alone in that. I might
be wrong, butut that said it needs to be investigated and in a really meaningful way to answer that,
before it becomes assume that acting hard and acting fast and all these b******t slogans are the truth
and they’d become the truth and they become fact. All without any really meaningful evidence
supporting them.
KK: I gotta say, I’ll get you Sumon next here, but I gotta say the idea of abandoning logic, I think that’s
that’s a key point there. Think about what we’re doing in restaurants, folks. Okay, you would literally
wear your mask to sit down, take off that bloody thing. Eat, chat, smooch even, I mean, and then put it
back on and go in the bathroom and think this is meaningful. Where’s the logic there? You’re on a plane,
you’re gonna drink something, you’re on a six hour flight, you know what I’m saying.
(?) During the lockdown, by the way, you’re sending like 20 Uber drivers to stand point. If you ever went
and picked up food, you would see these folks. It’d be like crowding the busy restaurants all like standing
in there, like arguing which orders theirs, you know what I mean? then like people waiting for the food
to show up.
KK: I mean, that’s the other point. The part that people forget with the lockdowns, tons of people will
work. I’m in Ottawa, where 70% are, could stay home, right? That’s a unique city. That’s why we were
very sheltered from this bad boy.
(?) Aren’t they still fighting going back to the office?
KK: Oh, my God. Folks, I’m sorry. Yeah, it’s like 70% could stay home, but you’re in GTA your area. That’s
a lot of essential workers. You don’t have that option. So, how’s this lockdown? Really looking at the big
picture? Anyway, sorry. Sumon you’re gonna hit it up.
SC: We just wanted to add one anecdote. I just think it kind of talks about all this is that, you know there
was a time when this thing started going to 2020. Stefan, I think you and I met online around that time.
You put a couple of seeds after I was reading stuff, like you know about the idea of, you know, risk
transfer risk being downloaded to other people. That’s sort of kind of think of a you know, what, like,
you know, a people that are working in the manufacturing industry, you’re not going to receive them a
lot unless you live in a place like Brampton or northwest Toronto, where the manufacturing hub of, of
Ontario and in many cases, central eastern Canada is right. So, I remember in, I was already starting to
use this doing anything. And when I was in, I guess it would have been the second wave when it was it
was pretty bad one, I just kept seeing factory worker after factory worker, but then the thing that stuck
out was tons of Amazon workers. So, I asked one of them, tell me something like, why are there so many
Amazon workers? Like are you guys? Is there a lot of sick people working that kind of thing? In
retrospect, it was very naive question. What that one woman told me that her face is burned into my
memory, she told me she goes, ‘Look, you know, every time a lockdown is called, or something happens
like that, what ends up happening is that the orders triple. So, then we end up working double and triple
shifts, and we all get COVID’ That was just a light went off. I was like, excuse my language, guys, but holy
s**t, we’re basically taking all this risk for people that can like what was it called a ‘laptop class’ that can
stay home and order all this stuff. Meanwhile, all that risk was going down to all these people, and I was
seeing it one, after another, after another, after another. I’m not sure if you guys saw that much, but I
was in Mississauga, that’s the hardest, Peele where the manufacturing industry is every single peanut
factory, the sheet metal, I just saw all of them. That I think was the kind of thing that turned me and
realize that we what we’ll be doing. I’ll shut up.
ZC: Yeah, I would say I mean, I think Stefan and Sumon make great points. You know, I think that that
was very apparent at the beginning. The other thing I would say is 2021 to 2022. Things like vaccination
and public health measures fell along political lines. That was a huge mistake. It was devastating. I
remember back to the first snap election in 2021. Initially great video of all the political parties
encouraging vaccination and putting their differences aside. Then all of a sudden, it became mudslinging
about how much public health measure you’re willing to do, how much you’re willing to invest in, and
it’s not a Canadian phenomenon. We saw this in the United States with the Biden and Trump campaigns
and the contrast between the two, and then really aligning public health views to political views, and
then, you know, really making it very uncomfortable for certain people to then express counter views
without being considered an alternative party. It’s something we need to reflect on I think we have
public health and public health messengers and people that are agnostic to political views but are really
there to support the health of their populations, from a health from a societal from an emotional from
the aspects of good health in that sense. You really can’t involve politics into that, because all of a
sudden, then you start getting counter current messaging, and you start getting people being pushed,
and you start new aligning values to views and you start saying, right and left based on what people
consider, where again, the science doesn’t necessarily follow political direction. It was a really big
mistake, and it still is pervasive. We saw every election that happened between 2021 to 2022 is public
health and public health messaging was embedded in each one of those and it caused more harm than
good. I think it’s a big lesson from this, this is that you can be proactive for effective public health
interventions as an individual in that society that has a role, but you can’t stick it on campaigns. It really
makes it hard to deescalate measures at that point when your campaign and your identity is tied to
certain public health measures in that sense.
KK: Amen. I am cognizant of the time and so I’m gonna try to rapid fire a little bit? I think, there’s only a
couple points that people hit up on that we haven’t touched on. There was a push for mass mandates in
the last couple months because of of RSV and influenza that was happening. It still is happening in,
especially in our extreme ages, really young and really old. Any viewpoint on that, I’ll leave it open to
almost to throw down.
(?) I think mass mandates have been useless. I don’t expect to ever folks to agree with me, it’s like it’s an
interesting dynamic, right? When you go and you saw folks who were on the buses, I take the bus to the
airport. Our subway in Toronto just for folks only starts at like, 5:50am. So, before that, you gotta jump
on buses. So the construction workers on the bus who were wearing masks during the when the mask
mandates were on taking this what’s called, it’s like the construction line, because it goes down Bloor
are basically and takes all the construction workers from Scarborough, before the subway line, get to
downtown to do all the construction and build all the stuff that you know, is being built right now.
Everyone is wearing this useless cloth mask. It’s like probably the one thing that the anti-maskers who I
think I probably am one at this point. The pro-maskers and all maskers can agree on is that cloth masks
are useless. That’s what 100% of these folks are wearing. They’re wearing these reusable cloth masks
that are like barely on their face often blow their nose. So, to me, it’s not so much about like, what could
this intervention achieve, if done perfectly like saying the study you were involved with the help lead,
it’s like everybody’s like, but all of them got COVID outside of the health care system, they didn’t get it
when they’re wearing their N95. That’s like, but that’s the point, like public health interventions live or
die or succeed or fail in the real world. I was seeing the real world, I would love to take a photo but I
don’t think these folks have been friendly to me taking a photo of them, but it was 100%, cloth masks of
all these folks in the morning all crowded, like we’re literally like person to person on this bus. It’s like a
perfect, you know, vehicle for massive transmission. I just I just sort of put that forward of like, that’s
what a mask mandate does to me. I think to the person sitting at home calling for them, they are just
imagining, they’re like ‘Oh but the government should do this’. But they didn’t. The government should
be handing out in N95’s. How are you going to police them wearing a N95’s and how are you getting
them? It would be so hard to make a massive program work. I would say it’s like if you gave me millions
and millions and millions of dollars, for me to design a mass program, I don’t know, maybe I could pull it
off you really with an endless budget. But for what? So, I just think that like as these programs went out
in the real world, I think they did nothing but burn people’s energy. You know because some people it
just turns out don’t like wearing a mask. Shocking to other folks. They just don’t like wearing a mask.
Last thing I’ll say is that just as they play it out in the real world, I think we’re functionally useless, other
than burning people’s energy. I’m a fervent anti masker at this point because it’s just an insult to public
health. To me everything I’ve trained in and everything I’ve worked towards, just saying these two words
mask mandate, as the fix. That is an insult to the very thing that I want to spend my life doing .
ZC: Yeah, I mean, three points, one: you know, masks are still important in clinical settings. I think we all
understand that. We’ve been doing them before we’ve been continuing to do them. So I you know,
that’s one piece. Second: I mean, to go with the point that was raised here, you know, the best study we
have is Bangladesh, right? 10% relative risk reduction. It’s interesting when you read the Bangladesh
study, because with community kind of people that pump up masking that are really trying to educate
and probably are also there to mask compliance. Mask’s compliance people, you get to 54% compliance,
when those people leave compliance drops significantly. Right. You know, I think you have to just look
around and see what happened in this last few months, regardless of the messaging. Maybe it’s the
communities I’m in, but I didn’t see mass compliance change significantly, maybe about 5%. In the
context of the last couple of months. You must understand the value of this public health intervention,
Bangladesh has actually a nice insight, not only into what we think the community based optimal
masking efficacy is, but also the fact that you really have to continue to enforce, enforce, enforce,
enforce, in order to get to that even 10%. Without that enforcement, you’re not getting anywhere in
that sense. That probably spells that it’s probably a very poor long term public health intervention in the
context that you really must pump it week by week by week by week in order to actually get compliance
that may actually then give you the effects that you see in a cluster randomized control trial. Again, you
know, the world we live in is showing that people don’t want to mask normally. Some people can, it’s a
good intervention for them, if they want to do it, I, we should respect everyone that wants to mask, I
think that the, on the other side, you know, people showing, you know, disdain, and making fun of
people who are masking in public. It is also something we need to address and really need to support
people in their medical decisions. At the same time, there’s a long-term effect of intervention. It’s not,
it’s not gonna be useful, because people don’t want to do it. And, you know, and the compliance issues
and everything else that comes from it. And, you know, the third thing I’ll say, is, with every mandate
comes with enforcement. What does enforcement look like? Is it that you can’t go to establishment X or
Y without a mask? If you’re someone who’s on the fringes with mental health issues with other issues,
are you going to doctors to get mask exemptions, right? So, you know, again, you then push people to
the fringes, you may not get the compliance you want and again, you may start then cracking down on
certain populations that that are disproportionately affected by types of mandates and rules in that
sense.
KK: 100%. Sumon
SC: You know, I heard a lot of good lines, in the last month or so, there’s something called the ‘No True
Scotsman’ fallacy. That very well applies to mask mandates, lock downs. It was it was cool, because I’ve
been hearing these all throughout the pandemic, and then it makes sense, is the ideas, or what if we did
the mask mandate, right? What Stefan was saying, if we masked hard enough, if we had just done this,
you know, that wasn’t a mask mandate. If we locked down hard to Oh, that wasn’t a lockdown. You
know, this is a lockdown. Obviously. Now, a lot of that stuff is ridiculous, because we’re three years out,
and we saw that even China, you saw what happened there, but no place ended up by being able to
completely keep it up, keep COVID away forever, so that the ‘No True Scotsman’ fallacy really applies. I
think that the insightful thing that I read, and actually might have been Twitter too, is that if you are
making a policy, and your explanation for why that policy didn’t work, is because people weren’t doing
it, right. There’s nothing, that doesn’t mean something wrong with the people, it means it’s a shitty
policy. I think that applies to any public policy, but for health ones, I think, especially at that that’s the
case.
SB: Yeah, I want to just finish, I want to pick up on something that Zain said, I’ve spent a big part of my
career looking at, like the role of police and laws in public health. Obviously, I’m white. So, I’m not gonna
sit here and say that I’ve lived experience around this, but it’s what one thing that we know is that like,
police interventions, or interventions that are based on using police don’t affect people that look like
me, they just don’t. I think what we saw in New York City very early was differential enforcement of like
masking laws, you see these videos of these aggressive police carrying guys off buses, slamming their
faces into the countertops. Then on the other side of the city in rich part of New York, the police are
walking around handing out masks to people ‘Hey, you should think about putting this on’ It’s the
differential enforcement that happens that says to me, like police serve an important role in society. I’m
not here to complain about the role of police. I think once you start relying on police, in public health,
like the whole thing is lost. You got to go back to the drawing board and start over. I think that like, our
alliance on police for the lockdown or alliance on police, and calling the police, as it related to mask is
for all of it meant that these were failed interventions, and particularly, again, affecting the very people
that we were expected to leave their homes that were getting more COVID. Then ended up on the
wrong end of the police related to these mandates, don’t go to public parks, when they don’t have
backyards. It was just so so strange and design and so counter to what I think Canada likes to think of
itself as ‘Canadian values’ and progressive values that I actually have a tough time coming to terms with
how it even happened and what worries me even more is that it’s gonna happen again.
KK: We lost our way. I’m just gonna straight up say we lost our way. When we when we let our fear run
our decisions as opposed to our values. This was when it was gone. As Canadians always figured, this is
what a place where we stick up for those that can’t stick up for themselves? It was I think that’s probably
where I had the hardest time. You mentioned how much this affected people that look like me or any
racialized communities like, this is a thing. This was like a beat down on racialized people like everything.
school closures, you know what I mean? You talk about vaccine passports. You mean like, Oh, let me
double check, let me triple check. I haven’t told anybody there’s a couple times in those restaurants,
where it’s like, double check, triple check. Let me make sure that second dose was there, like, I’m gonna
really check and make sure that this is a valid vaccine passport. Lockdowns? Who’s the essential
workers? I think we were okay with all this stuff because it didn’t affect the most, more racialized
people, the people that didn’t have as much of a voice. This is what pissed me off, frankly. That it was
okay, that we were, whether it was you know, racialized community, whether it was kids, people that
were vulnerable, and they can’t speak up for themselves, like, that’s who we justified and said, Okay,
we’ll just keep doing what we’re doing, despite the data, despite the data showing, like whether it’s
effective or not. Whether you’re looking at BC or Ontario that does completely different approaches,
with the same results in the same country. This is what are people were doing, I gotta say it like it, just, it
just eat at me. Second point, I’ll make one before going to Stef is, I think you may also good point about
the investment, like people have a certain amount of bandwidth in general, you’re gonna say let’s mask
harder, let’s duel these event interventions harder. One thing that As always, this was on a thicket,
another live cast, that we did stuff, but when you said, let’s focus on interventions, as opposed to
restrictions, let’s invest there, that makes so much sense to me. Especially when you know areas that
are going to be the hardest hit when you know, where were the most vulnerable. Let’s invest there, put
the vaccines there, offer paid leave there, invest, where it’s gonna give you the biggest bang for your
buck. That to me, like if you think about all the money spent, wow. To have infrastructure to, to be able
to handle future pandemics like that point to, I think we can’t overlook that, you know, when you invest
more time and effort into areas that are less effective, you know, it’s a distraction, it really, it really can
be a distraction. Anyway, Stef
SB: I just want to say that the last thing I would want for our province or our cities or our hospitals to
release just one data point, one data point. We often talk about, they’re like, oh, in the end, it was only a
few percent of people fired related to vaccine mandates. You know, I would just love them to release
the demographics of who was fired. We know that there’s like a lot of historical mistrust for it, by the
way, good reason I meet a lot of people with like, I always think like a patient’s making a rational
decision, based on their own dynamic, their own history, most people are making rational decisions, it
might not be the decision I want them to make. It might not be the absolute, but it is like the right
decision for themselves. Sometimes that decision was not to get vaccinated. I would just love for people
to release that for the City of Toronto, the City of Ottawa, the province of Ontario to just release data on
on our hospitals, what were the demographics of the people who were fired. My guess is just from what
I’ve seen, it’s going to look really ugly in terms of people who say that they’re supportive of particularly
racialized communities. So, I think that’s part of it is that you can’t overcome medical mistrust. In a five-
minute conversation, you can’t just be like, ‘Oh, trust me, now. I’m here to fix it now. Like, I know, like,
generations have lied to you. But like, I’m, you could trust me now’ I mean you can’t you can’t just fix
that. Anyways, I just think that that’s gonna be an important statistic. Otherwise, again, like, in a few
years, I think the next pandemic that easily be in the next 5 to 10 years, so you know we’re gonna be
back here with vaccine mandates, lock downs, etc. Unless we’d like, more meaningfully explore what
happened.
KK: Yeah. Thank you for that point. I must say this is a follow up. I do some talks on systemic racism.
George Floyd was a part of that, but it was also seeing who was getting hardest hit throughout the
pandemic. I hate giving those talks because it’s like, it’s, you know, if I’m being honest, it’s a bit
traumatic. You put yourself in a vulnerable spot talking about You know, tough times, but I think, you
know, this was another area that we just need to recognize that this is not this is not an equal problem.
This is not a problem that’s just hits up everyone equally, it really those that are racialized, it hits the
most. I’m cognitive of the time. So, I think we’re gonna, we’re gonna wind up here. I just want to make a
couple final points. I think, one: I really hope in the future that we, we learn about the negative impacts
of having a fear narrative, like we want to be able to create trust, moving forward with public health
with, and I really, truly, humbly believe that when we have that fear narrative, when we make decisions
from a place of fear that pulls us further away, pulls us further away from our values and, and making
correct decisions that decisions that will be more holistic. So that’s one point I want to close on. The
second is: I think value of having this conversation, like a lot of people approach, I’m sure you guys get
this approach us talking about how having that kind of balanced view has been so valuable throughout
and having the conversation right now about, you know, where we’ve, where we, where we could have
done better, I honestly feel like it’s healing for a lot of people. When we talk about things that weren’t
logical, their approaches that seem to, we’re doing these things that didn’t make sense. ‘I was trying to
do the right thing, they told me after three vaccines that we’d be no more locked down, yet we locked
down’ a lot of people who are looking for validation for the things that they’ve gone through. I think
having conversations like this validates things, it also gives them hope that that the future we all of us
are leaders that are on this panel with people that like us that are being able to have a voice can really
advocate for a better future when it comes to next time a pandemic like this happens. I want to thank
our panelists, because I really think these conversations will make a difference, like many of the stuff
that we’ve done over the last few years clinically, from an information point of view, or a
communication point of view, it makes a difference. So, I want to thank Zain, Sumon, Stef for such a
great conversation, as usual. So, thank you, thanks for those that are that joined on Facebook. Once
again, put NL in the in the chat box and you’ll get a copy of this or, or subscribe to our Substack and
you’ll get a version of this video and the audio. We really appreciate you guys signing in and you will not
see us hopefully for a very, very long time. All right, folks, thanks so much.
Get full access to Solving Healthcare Media with Dr. Kwadwo Kyeremanteng at kwadcast.substack.com/subscribe